Heterotopic Ossification after Acetabular Fractures: Prevention and Management
Vol 1 | Issue 1 | Jan-Apr 2016 | page: 20-22 | Rohit Jain[1].
Author: Rohit Jain[1].
[1] Sancheti Institute of Orthopedics and Rehabilitation,Pune, India.
Address of Correspondence
Dr. Rohit Jain
Sancheti Institute of Orthopedics and Rehabilitation,Pune, India.
Email : rj2april@gmail.com
Abstract
Background: Heterotopic ossification is a common complication after acetabular fractures that causes limitation of movements and functional disability. The aetiopathogenesis remains doubtful with various risk factors being described to be associated with it like associated brain injury, extensile approaches,male sex . The role of NSAIDS especially indomethacin and radiotherapy have been described for the prevention and management of heterotopic ossification. However there is no general consensus with few studies refuting their role. The purpose of this review is to discuss the prevention and management of heterotopic ossification and the associated side effects of indomethacin and radiotherapy.
Keywords: Heterotopic ossification, acetabular fractures, indomethacin, radiotherapy.
Introduction
Heterotopic ossification after acetabular fractures is one of the most common complications, the incidence being from 5 % to 100%.(1-10) The occurrence of heterotopic ossification lead to severe restriction of range of motion that leads to severe decrease in the functionality of the patient.
Pathophysiology
Heterotopic ossification is divided into 3 types based upon the aetiology – (a)Neurological, (b) genetic and (c) traumatic(11). But the pathophysiology still remains doubtful. Numerous factors such as Prostaglandin activity, especially PGE-2, hypercalcemia, sympathetic dysfunction,prolonged immobilization and imbalance between PTH activity and calcitonin have been implicated contributing to the formation of heterotopic ossification. The primitive mesenchymal cells in the surrounding soft tissues are converted into osteoblastic cells due to these factors(12).This differentiation of the mesenchymal cells into osteoblastic cells starts within 16 hours of surgery with peak at 32 hours after surgery(13). Since the exact aetiopathogenenis is still doubtful, various risk factors have been found to identify patients at risk for this complication(1-3,5,14-19). This risk factors are
1. The type of approach – Extended Iliofemoral approach – highest risk, Kocher-Lagenback approach – intermediate risk, Ilioinguinal approach – lowest risk. Complex approaches, trochanteric osteotomy and double exposures are also associated with increased risk of heterotopic ossification
2. Male sex
3. Associated traumatic brain injury or thoraco-abdominal inury
4. T – type acetabular fracture and associated injuries such as sciatic nerve injury,femoral head injury, intraarticular debris
5. Delayed surgery.
Recent articles have found conflicting results in terms of risk factors [20,21]. These studies reported that age, gender, injury severity score (ISS), presence of neurologic injury, occurrence of hip dislocation, interval from injury to surgery, presence of comminution, femoral head impaction, debris in the joint, number of other fractures, and head and chest did not correlated with formation of HO. One study reported prolonged mechanical ventilation as a risk factor [21] while the other reported length of stay in intensive care and non-intensive care length of stay in the hospital [20] to significantly affect the HO rates. This may be because both these studies used either indomethacin and radiotherapy for prophylaxis which reduces the risk significantly even in presence of other risk factors.
Classification
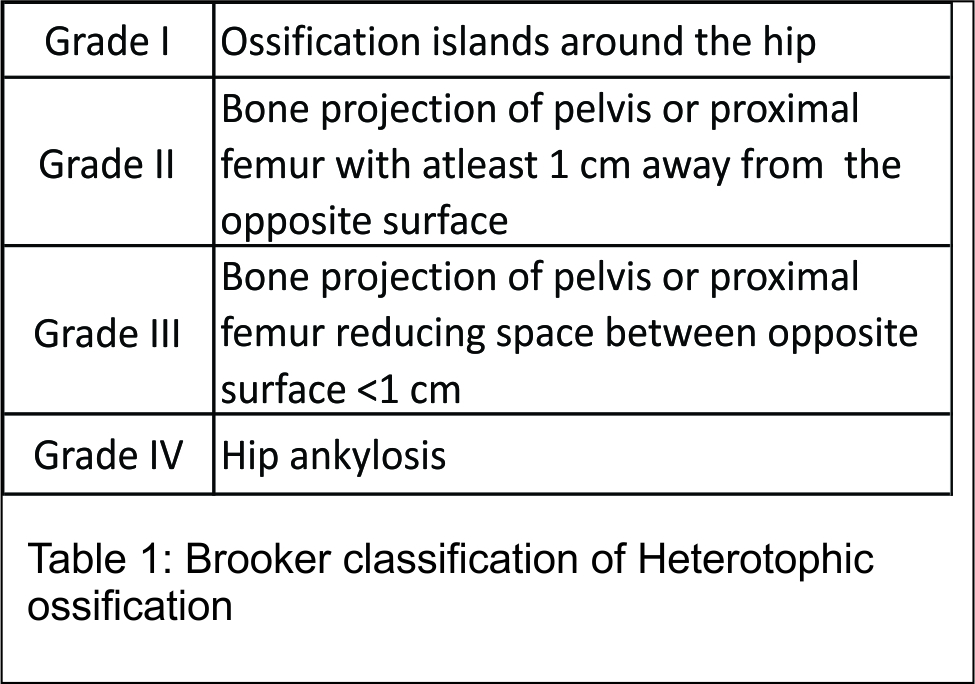
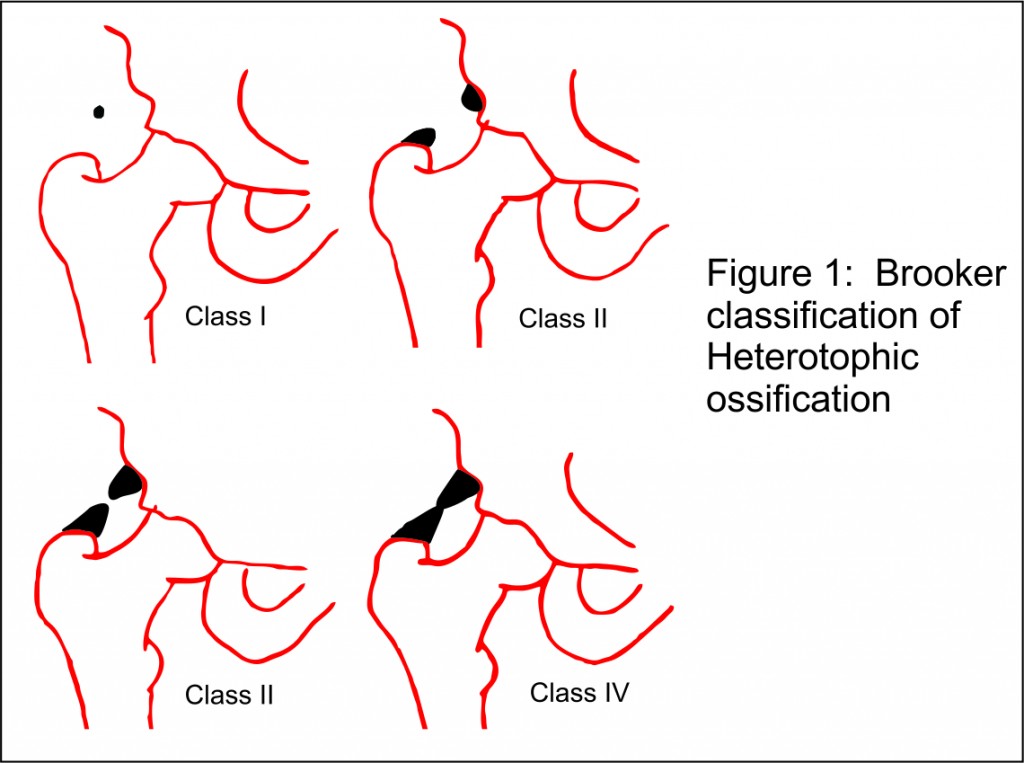
Brooker et al (22) classified heterotopic ossification around hip into 4 types radiographically based upon AP view of pelvis with both hips (Table 1, Fig 1).
Della Vale (23) modified the Brooker classification based upon routine AP pelvis with both hips x ray and additionally inlet and outlet Judet oblique views
· Grade A: absence of HO (may be ≥1 island of bone of <1 cm in length
· Grade B: presence of ≥1 islands of bone of at least 1 cm in length and bone spurs from the pelvis or femur. 1 cm distance between opposing surfaces of bone
· Grade C: bone spurs arising from the pelvis or femur with <1 cm between opposing surfaces or apparent bone ankylosis.
Prevention
Prophylactic indomethacin (13,14,20)and sProphylactic indomethacin (15,16,24)and single dose radiotherapy(25,26) have been used for the prevention of heterotopic ossification.
1. Indomethacin is used in dose of 25mg three times a day or 75mg sustained release immediately after surgery usually within 24- 48 hours for 7 -14 days. Amongst all the NSAIDS, only indomethacin has been found to have evidence in prevention of heterotopic ossification(22). Sagi et al (27) compared the efficacy of indomethacin given for 3 days,7 days and 6 weeks versus placebo in prevention of heterotopic ossification and found best results in indomethacin given for 7 days and worst results when indomethacin was given for 6 weeks. But Karunakar et al in their double blinded RCT found no significant difference in the formation of heterotopic ossification between the placebo group and indomethacin group(7). They suggested risk stratification and improved surgical technique will be enough to bring down the HO rates.
Mechanism of action: Inhibition of PGE-2 mediated bone remodeling and differentiation of osteoprogenitor cells (28,29).
Side-effects: prolonged bleeding time, gastro-intestinal irritation, impaired fracture healings, renal toxicity (29).
2.Radiotherapy in form single dose of 700 to 800 Cgy is given prophylactically for prevention of heterotopic ossification(30).
Mechanism of action: prevent formation of heterotopic ossification by disrupting the mesenchymal cells (25,30).
Side-effects: Increased risk of malignancy, oligospermia, high cost(31).
The surgical technique also plays a role in the prevention of heterotopic ossification. Routt and Swiontkowski recommended debridement of necrotic gluteus minimus muscle to reduce the risk of heterotopic ossification (17). Other have suggested that gluteus minimus debridement with single dose of radiation will be enough to bring the HO rates to minimum [32]. Careful surgical technique in form of protection of abductors, debridement of necrotic gluteus minimus and digastric slide osteotomy may also reduce HO rates [33]. Combined approach using radiation and Indomethacin has been used in high risk total hip replacement but its use in acetabular surgery in not reported. Combined use of improved surgical techniques and reduce dose of radiation/indomethacin may be the best combination, but requires further investigation. Radiation has been reported to be safer than Indomethacin but cost is much higher [34]
Management
The initial management consists of investigating for other sources of pain such as infection, neuroma, post traumatic arthritis followed by physiotherapy for improving the range of motion and NSAIDs. The NSAIDs provide relief from pain and reduce inflammation but do not prevent or inhibit new bone formation. Finally, the only treatment option of already formed heterotopic ossification is delayed surgical excision of the ossified mass which is usually done after 6 months postoperatively when it is encapsulated followed by secondary prophylaxis to prevent recurrence(35). Recent article by Wu et al [36] based the surgical excision on alkaline phosphatase (ALP) level and not on duration after fixation. They believe ALP to be much more sensitive indicator of HO maturity. They suggested early surgical removal of HO [surgery > 3 months and ALP levels normal] rather than waiting for 9-12 months. The surgery itself has complication like femoral neck fracture, sciatic nerve injury, AVN and around 33% recurrence rate was reported by them. Thus proper selection of patient and assessment of risk – benefit ratio should be taken into account before undertaking surgical exercise.
Conclusion
Enough evidence exist to justify routine usage of prophylaxis to prevent heterotrophic ossification in surgical management of acetabular fracture. Although randomised trial exists but superiority of either of the methods viz indomethacin or radiation therapy is not firmly established and either can be used as per availability, surgeons preference or institute protocols. Optimised surgical technique and debridement of necrotic gluteus minimus will help in further reducing the incidence
Clinical Message
HO is a common occurrence but mild to moderate HO may not significantly affect outcome. A risk assessment of HO and appropriate prophylaxis plan using either Indomethacin or radiation will prevent severe HO in most patients. Improved surgical technique and safe tissue handling will further reduce the incidence. In case with established HO, surgical excision is an option it the assessment of risk benefit ratio is favorable.
References
1. Alonso J, Davila R, Bradley E. Extended iliofemoral versus triradiate approaches in management of associated acetabular fractures. Clin Orthop Relat Res. 1994;305:81–87.
2. Bray T, Esser M, Fulkerson L. Osteotomy of the trochanter in open reduction and internal fixation of acetabular fractures. J Bone Joint Surg Am. 1987;69:711–717
3. Daum W, Scarborough M, Gordon W, Uchida T. Heterotopic ossification and other perioperative complications of acetabular fractures. J Orthop Trauma. 1992;6:427–432.
4. Ebraheim N, Patil V, Liu J, Haman S. Sliding trochanteric osteotomy in acetabular fractures: a review of 30 cases. Injury. 2007;38:1177–1182.
5. Ghalambor N, Matta J, Bernstein L. Heterotopic ossification following operative treatment of acetabular fracture. An analysis of risk factors. Clin Orthop Relat Res. 1994;305:96–105.
6. Griffin D, Beaule P, Matta J. Safety and efficacy of the extended iliofemoral approach in the treatment of complex fractures of the acetabulum. J Bone Joint Surg Br. 2005;87:1391–1396.
7. Karunakar MA, Sen A, Bosse MJ, Sims SH, Goulet JA, Kellam JF. Indomethacin as prophylaxis for heterotopic ossification after the operative treatment of fractures of the acetabulum. J Bone Joint Surg Br. 2006;88:1613–1617.
8. Heck B, Ebraheim N, Foetisch C. Direct complications of trochanteric osteotomy in open reduction and internal fixation of acetabular fractures. Am J Orthop (Belle Mead NJ). 1997;26:124–128.
9. Heeg M, Klasen H, Visser J. Operative treatment for acetabular fractures. J Bone Joint Surg Br. 1990;72:383–386.
10. Johnson E, Kay R, Dorey F. Heterotopic ossification prophylaxis following operative treatment of acetabular fracture. Clin Orthop. Relat Res. 1994;305:88–95.
11. Board TN, Karva A, Board RE, Gambhir AK, Porter ML: The prophylaxis and treatment of heterotopic ossification following lower limb arthroplasty. J Bone Joint Surg Br 2007, 89:434-440.
12. Shehab D, Elgazzar AH, Collier BD: Heterotopic ossification. J Nucl Med 2002, 43:346-353
13. Tonna EA, Cronkite EP. Autoradiographic studies of cell proliferation in the periosteum of intact and fractured femora of mice utilizing DNA labeling with H3-thymidine. Proc Soc Exp Biol Med. 1961;107:719–21.
14. Johnson E, Kay R, Dorey F. Heterotopic ossification prophylaxis following operative treatment of acetabular fracture. Clin Orthop Relat Res. 1994;305:88–95.
15. Matta J, Siebenrock K. Does indomethacin reduce heterotopic bone formation after operations for acetabular fractures? J Bone Joint Surg Br. 1997;79:959–963.
16. Moed B, Karges D. Prophylactic indomethacin for the prevention of heterotopic ossification after acetabular fracture surgery in high-risk patients. J Orthop Trauma. 1994;8:34–39.
17. Routt MJ, Swiontkowski M. Operative treatment of complex acetabular fractures. Combined anterior and posterior exposures during the same procedure. J Bone Joint Surg Am. 1990;72:897–904
18. Starr A, Watson J, Reinert C, Jones A, Whitlock S, Griffin D, Borer D. Complications following the ‘T extensile’ approach: a modified extensile approach for acetabular fracture surgery—report of fortythree patients. J Orthop Trauma. 2002;16:535–542.
19. Webb L, Bosse M, Mayo K, Lange R, Miller M, Swiontkowski M. Results in patients with craniocerebral trauma and operatively managed acetabular fracture. J Orthop Trauma. 1990;4:376–382
20. Firoozabadi R, O’Mara TJ, Swenson A, Agel J, Beck JD, Routt M. Risk factors for the development of heterotopic ossification after acetabular fracture fixation. Clin Orthop Relat Res. 2014 Nov;472(11):3383-8
21. d’Heurle A, Archdeacon MT, Hiratzka S, Casstevens C, Finnan R, McCoy B. Do Surrogates Of Injury Severity Influence The Occurrence Of Heterotopic Ossification In Fractures Of The Acetabulum? J Orthop Trauma. 2015 Nov 16.
22. Brooker A, Bowerman J, Robinson R, Riley LJ. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973;55:1629–1632.
23. Della Valle AG, Ruzo PS, Pavone V, Tolo E, Mintz DN, Salvati EA. Heterotopic ossification after total hip arthroplasty: a critical analysis of the Brooker
Oct;17(7):870-5.
24. Macfarlane RJ, Ng BH, Gamie Z, El Masry MA, Velonis S, Schizas C, et al. Pharmacological treatment of heterotopic ossification following hip and acetabular surgery. Expert Opin Pharmacother. 2008;9(5):767–86
25. Anglen JO, Moore KD. Prevention of heterotopic bone formation after acetabular fracture fixation by single-dose radiation therapy: a preliminary report. J Orthop Trauma. 1996;10:258–263.
26. Childs HA 3rd, Cole T, Falkenberg E, Smith JT, Alonso JE, Stannard JP, Spencer SA, Fiveash J, Raben D, Bonner JA, Westfall AO, Kim RY. A prospective evaluation of the timing of postoperative radiotherapy for preventing heterotopic ossification following traumatic acetabular fractures. Int J Radiat Oncol Biol Phys. 2000;47:1347–1352.
27. Sagi HC, Jordan CJ, Barei DP, Serrano-Riera R, Steverson B. Indomethacin
prophylaxis for heterotopic ossification after acetabular fracture surgery
increases the risk for nonunion of the posterior wall. J Orthop Trauma.
2014;28(7):377–83.
28. Banovac K, Williams JM, Patrick LD, Haniff YM: Prevention of heterotopic ossification after spinal cord injury with indomethacin. Spinal Cord 2001, 39:370-374.
29. Burd TA, Hughes MS, Anglen JO: Heterotopic ossification prophylaxis with indomethacin increases the risk of long-bone non-union. J Bone Joint Surg Br 2003, 85:700-705.
30. Ayers DC, Evarts CM, Parkinson JR. The prevention of hetero-topic ossification in high-risk patients by low-dose radiation therapy after total hip arthroplasty. J Bone Joint Surg Am.1986;68:1423–1430.
31. Burd TA, Lowry KJ, Anglen JO. Indomethacin compared with localized irradiation for the prevention of heterotopic ossification following surgical treatment of acetabular fractures. J Bone Joint Surg Am. Dec; 2001 83-A(12):1783–1788.
32. Davis JA, Roper B, Munz JW, Achor TS, Galpin M, Choo AM, Gary JL. Does Postoperative Radiation Decrease Heterotopic Ossification After the Kocher-Langenbeck Approach for Acetabular Fracture? Clin Orthop Relat Res. 2015 Oct 23
33. Griffin SM, Sims SH, Karunakar MA, Seymour R, Haines N. Heterotopic ossification rates after acetabular fracture surgery are unchanged without indomethacin prophylaxis. Clin Orthop Relat Res. 2013 Sep;471(9):2776-82.
34. Burnet NG, Nasr P, Yip G, Scaife JE, House T, Thomas SJ, Harris F, Owen PJ, Hull P. Prophylactic radiotherapy against heterotopic ossification following internal fixation of acetabular fractures: a comparative estimate of risk. Br J Radiol. 2014 Oct;87(1042):20140398.
35. Thomas BJ. Heterotopic bone formation after total hip arthroplasty. Orthop Clin North Am. 1992;23(2):347–58
36. Wu XB, Yang MH, Zhu SW, Cao QY, Wu HH, Wang MY, Cuellar DO 3rd, Mauffrey C. Surgical resection of severe heterotopic ossification after open reduction and internal fixation of acetabular fractures: a case series of 18 patients. Injury. 2014 Oct;45(10):1604-10.
| How to Cite this article: Jain R. Heterotopic Ossification after Acetabular Fractures: Prevention and Management. Journal of Orthopaedic Complications Jan-April 2016; 1(1):20-22. |