Recurrent Pseudomeningocele Following Surgery for Cervical Intramedullary Subependymoma: A Complex Case Report
Case Report | Vol 2 | Issue 3 | September-December 2025 | page: 28-32 | Arvind Vatkar, Sachin Kale, Aniket Sonawane
Submitted Date: 05-06-2025, Review Date: 13-07-2025, Accepted Date: 04-09-2025 & Published Date: 10-12-2025
https://doi.org/10.13107/joc.2025.v02.i03.40
Authors: Arvind Vatkar [1], Sachin Kale [2], Aniket Sonawane [1]
[1] Department of Orthopaedics, MGM Medical College, Nerul, Navi Mumbai, Maharashtra, India.
[2] Department of Orthopaedics, DY Patil Medical College, Nerul, Navi Mumbai, Maharashtra, India.
Address of Correspondence
Dr. Arvind Vatkar
Assistant Professor, Department of Orthopaedics, MGM Medical College, Nerul, Navi Mumbai, Maharashtra, India.
Email: vatkararvind@gmail.com
Abstract
Pseudomeningocele (PMC) is a rare complication of cervical spine surgery, typically manifesting as an abnormal cerebrospinal fluid (CSF) collection in the paraspinal tissues. We present a unique case of a 39-year-old male who developed recurrent symptomatic pseudomeningocele following surgical excision of a C5-T1 intramedullary subependymoma. The patient initially presented with progressive weakness in the lower limbs and upper motor neuron signs. Following primary tumor excision and fixation (C5-T1 laminectomy, excision, biopsy, and fusion on 20.02.2023), the patient developed postoperative pseudomeningocele with significant neurological deficit. Revision surgery for pseudomeningocele repair was performed, yet the collection persisted. Despite persistent CSF collection on imaging, the patient showed progressive neurological recovery with conservative management including acetazolamide therapy and physiotherapy. The patient now demonstrates substantially improved motor power with residual symptoms of postural headaches and giddiness. This case highlights the variable clinical course of pseudomeningocele and the potential for neurological recovery despite persistent imaging findings, as well as the effectiveness of conservative management with pharmacological and rehabilitative interventions.
Keywords: Pseudomeningocele, Intramedullary tumor, Cervical spine surgery, Subependymoma, CSF leak, Acetazolamide
Introduction
Pseudomeningocele (PMC) represents an abnormal collection of cerebrospinal fluid (CSF) that communicates between the subarachnoid space and the paraspinal soft tissue [1]. Although PMC is a well-recognized complication of posterior cervical spine surgery, it remains relatively uncommon following anterior decompression procedures. The reported incidence of PMC in the general cervical spine surgery population ranges from less than 0.1% to 0.5% [1, 3].
PMC can result in various clinical manifestations, including pain, headaches, nerve root entrapment, and in rare cases, spinal cord compression [1]. The clinical presentation typically depends on the size and location of the fluid collection, as well as the degree of neural element involvement [2]. Conservative management is often successful for asymptomatic cases, whereas symptomatic pseudomeningoceles warrant more aggressive intervention, including lumbar drainage, shunting procedures, and/or direct surgical repair of the dural defect [1, 2].
Intramedullary tumors of the spinal cord, particularly subependymomas, represent a specific subset of spinal pathology. Subependymomas are WHO Grade I tumors that typically have a slow growth rate and favorable prognosis when appropriately managed surgically [4]. However, the surgical management of these lesions carries inherent risks of dural violation and subsequent CSF leakage, which can precipitate pseudomeningocele formation.
We present a complex case of recurrent symptomatic pseudomeningocele following surgical treatment of a C5-T1 intramedullary subependymoma, with an unusual clinical course characterized by persistent imaging findings despite progressive neurological recovery on conservative management.
Case Presentation
Patient Demographics and Initial Presentation
A 39-year-old male presented with a one-year history of progressive weakness in the right hand and tremors. The patient also reported progressive spasticity in the bilateral lower limbs over the preceding 2-3 years. There was no history of trauma, fall, fever, or constitutional symptoms. Clinical examination revealed upper motor neuron signs with intact motor power at the time of initial presentation.
Magnetic resonance imaging (MRI) of the cervical spine revealed an ill-defined intramedullary mass lesion at the C5-T1 level, measuring approximately 34 mm in anteroposterior dimension. The radiological findings were consistent with an intramedullary space-occupying lesion, likely representing a subependymoma.
Initial Surgical Intervention
On 20.02.2023, the patient underwent surgical treatment consisting of C5-T1 laminectomy, tumor excision, biopsy, and fixation under general anesthesia at the Institute of Neurosciences, Kolkata. Intraoperative findings included difficulty in engulfing the nerve root due to tumor adherence, which was managed during tumor capsule dissection. The tumor was completely excised, and histopathology confirmed the diagnosis of Grade I subependymoma.
The immediate postoperative course was uneventful, and the patient was mobilized with physiotherapy.
Postoperative Complication: Pseudomeningocele Development
Approximately six weeks post-tumor excision (April 2023), the patient presented with complaints of swelling at the nape of the neck, neck pain, and progressive weakness of the left hand grip. Clinical examination at this stage revealed:
• Upper Limb Motor Power (C5-T1 distribution):
• Left side: 2/5
• Right side: 3/5
• Lower Limb Motor Power: 3/5 (bilateral)
• Associated Signs: Palpable swelling at the nape of neck
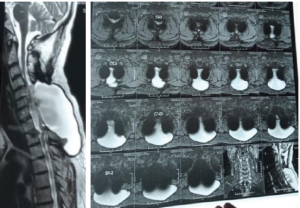
Postoperative MRI cervical spine (17.11.2025) demonstrated:
• Extra-dural CSF-like intensity fluid collection measuring approximately 122 × 51 × 75 mm (previously 119 mm × 94 mm × 115 mm on prior imaging)
• The collection arose from a postoperative dural defect extending from C5 to T1 vertebral levels
• The fluid extended into the posterior subcutaneous tissues of the neck, reaching the level of T3 vertebra
• Posterior displacement of the spinal cord extending from C5 to D1 levels
• Spinal cord appeared adherent to the posterior dura with flattening, marked thinning, and T2 hyperintensity
• Radiological findings consistent with dorsal cord herniation with myelomalacia
• Mild associated syringomyelia noted at C3-C4 level
• Posterior disc osteophytes at C4-C5 and C5-C6 levels with mild spinal canal narrowing
The imaging findings confirmed the diagnosis of pseudomeningocele arising from a postoperative dural defect.
Initial Management and Revision Surgery
Following diagnosis, the patient underwent multiple interventions for pseudomeningocele management:
First Intervention (April 2023):
1. Lumbar drain placement at L4-L5 interspace under general anesthesia on 20.04.2023
2. Drain repositioning was performed
3. Drain removal on 27.04.2023
Second Intervention (April 2023):
• Wound exploration and repair performed under general anesthesia on 25.04.2023
Third Intervention (April-May 2023):
1. Lumbar drain re-placement at L4-L5 interspace under local infiltration with 2% lignocaine on 30.04.2023
2. Drain removal on 03.05.2023
Clinical Course and Current Status
Despite multiple revision interventions, MRI imaging continues to demonstrate persistent pseudomeningocele with mild size reduction (122 × 51 × 75 mm compared to previous 119 mm × 94 mm × 115 mm) as shown in figure 1. THe patient also has a palpable fluctuant swelling in his cervicodorsal region in midline as shown in figure 2. However, the patient has demonstrated progressive neurological recovery over the follow-up period. (Fig. 1, 2)

Current Motor Status (Approximately 6 month post-revision surgery):
• C5-T1 Distribution Left Upper Limb: 4/5
• Right Upper Limb: 5/5
• Lower Limbs (bilateral): 5/5
Persistent Symptoms:
• Postural headaches occurring after prolonged sitting
• Giddiness with episodes of falling when standing up from squatting position
• These symptoms suggest possible intracranial hypotension or postural orthostatic tachycardia
Current Management:
• Acetazolamide (carbonic anhydrase inhibitor) – typically dosed at 250 mg twice daily
• Intensive physiotherapy and rehabilitation
• Regular neurological monitoring
The patient is being managed conservatively with good compliance to medical therapy and rehabilitation protocols.
Discussion
This case presents several interesting clinical and management challenges related to pseudomeningocele following intramedullary tumor excision.
Pseudomeningocele in Spinal Tumor Surgery
The development of pseudomeningocele following spinal surgery is a recognized complication, though reports specifically following intramedullary tumor excision are relatively limited in the literature [1, 2, 3]. The incidence of CSF leakage complications varies depending on the surgical approach and the underlying pathology. In contrast to ossification of the posterior longitudinal ligament (OPLL) surgery, where dural violation rates are reported between 4.3-32%, pseudomeningocele following intramedullary tumor surgery has not been precisely quantified [5, 6].
The mechanism of pseudomeningocele formation involves a defect in the dural-arachnoid layer, allowing CSF to extravasate into the surrounding soft tissues where it becomes sequestered by the inflammatory and fibrous tissue response [1]. In this patient, the dural defect likely occurred during tumor dissection, possibly related to the difficulties encountered during nerve root management due to tumor adherence.
Clinical Presentation and Imaging Features
The clinical presentation of this pseudomeningocele was characterized by progressive motor deficit in the immediate postoperative period, with particular involvement of the C5-T1 distribution bilaterally. The imaging findings were notable for the large size of the collection (122 × 51 × 75 mm), its communication with the spinal CSF spaces, and its extension into the subcutaneous tissues extending to the T3 level.
Of particular interest was the radiological demonstration of dorsal cord herniation with myelomalacia, which likely explained the acute neurological deterioration experienced postoperatively. The cord appeared adherent to the dural defect, and the T2 hyperintensity suggested areas of cord edema or ischemic change secondary to compression and cord displacement [2].
Management Approach and Treatment Rationale
Multiple management strategies were employed in this case, reflecting the complex nature of recurrent pseudomeningocele:
Lumbar Drainage: Initial lumbar drain placement was performed to reduce the CSF pressure gradient across the dural defect, theoretically allowing the defect to heal by reducing CSF extravasation [1, 2]. The temporary nature of this intervention (drained for 6-8 days at a time) made it suitable as an initial trial of non-operative management.
Surgical Repair: Wound exploration and repair was undertaken with the goal of directly addressing the dural defect. However, the persistence of the pseudomeningocele despite this intervention suggests either incomplete defect closure or reformation of the dural defect.
Acetazolamide Therapy: The use of acetazolamide in the chronic management phase is of particular interest. Carbonic anhydrase inhibitors reduce CSF production by acting on the choroid plexus and reducing aqueous humor production in the eye by similar mechanisms [7]. The pharmacological reduction of CSF production may reduce the pressure gradient driving CSF through the dural defect, thereby promoting defect healing. This approach has been reported in the management of persistent CSF leaks and represents a conservative option for preventing the need for repeat surgical intervention [7].
Physiotherapy and Rehabilitation: The intensive physiotherapy and neurological rehabilitation likely contributed significantly to the neurological recovery demonstrated by this patient. Progressive motor recovery despite persistent imaging findings suggests that the initial spinal cord compression and displacement were partially reversible, and that the CSF collection itself may not have remained massively compressive despite its persistent presence on imaging.
Discordance between Imaging and Clinical Findings
A notable feature of this case is the apparent discordance between persistent imaging findings (pseudomeningocele collection size) and progressive clinical improvement. This phenomenon has been described in other CSF leak complications and likely reflects several factors:
1. Organization of fluid collection: Over time, the CSF collection becomes increasingly organized and loculated by fibrous tissue, reducing its mass effect even if the volumetric size remains similar [1].
2. Cord plasticity: Spinal cord tissue may gradually reorganize and adapt to chronic compression, particularly when the compression develops gradually over weeks to months [8].
3. Arachnoid barrier: Progressive fibrosis of the dural-arachnoid interface may contain the collection more effectively over time.
Postural Symptoms and Intracranial Hypotension
The persistent postural headaches and giddiness with positional symptoms suggest an element of CSF hypotension or autonomic dysfunction. Patients with chronic CSF leaks may develop intracranial hypotension symptoms that persist despite stabilization or reduction of the CSF collection [1]. The orthostatic nature of the symptoms (particularly triggered by transitions from squat or sitting positions) is highly suggestive of postural orthostatic tachycardia or cerebral hypoperfusion related to intracranial hypotension.
Acetazolamide has dual benefits in this context: it reduces CSF production while simultaneously increasing cerebral blood flow through vasodilatory effects, potentially addressing both the CSF dynamics and the hemodynamic aspects of the patient’s symptoms [7].
Conclusion
This case of recurrent pseudomeningocele following intramedullary subependymoma excision demonstrates the variable clinical course of this complication and the potential for neurological recovery despite persistent imaging abnormalities. While traditional management of symptomatic pseudomeningocele has emphasized surgical repair of the dural defect, this case illustrates that conservative management incorporating CSF production reduction (acetazolamide), aggressive rehabilitation, and careful neurological monitoring can result in substantial functional improvement.
The persistent postural symptoms suggest ongoing CSF dynamics abnormalities that warrant continued monitoring and symptom-directed management. Future cases should explore the long-term efficacy of acetazolamide-based conservative management in recurrent or persistent pseudomeningoceles as an alternative to repeated surgical intervention.
Although pseudomeningocele remains a challenging complication of spinal surgery, the combination of pharmacological intervention targeting CSF physiology, intensive rehabilitation, and patient education regarding symptom management offers a reasonable approach for selected cases with persistent but non-progressive neurological deficit.
References
[1] Ailon T, Smith JS, Nassr A, et al. Rare complications of cervical spine surgery: pseudomeningocoele. Global Spine Journal. 2017;7:109S-14S. doi:10.1177/2192568216687769
[2] Tzerefos C, Paterakis K, Bouramas D, et al. Late-Onset Cervical Pseudomeningocele Following Ossification of the Posterior Longitudinal Ligament Surgery Successfully Treated With a Lumboperitoneal Shunt. Cureus. 2022;14(10):e30744. doi:10.7759/cureus.30744
[3] Helle TL, Conley FK. Postoperative cervical pseudomeningocele as a cause of delayed myelopathy. Neurosurgery. 1981;9:314-316.
[4] Chamberlain MC. Spinal cord gliomas: a review. Journal of Neuro-Oncology. 2009;47(3):231-238.
[5] Belanger TA, Roh JS, Hanks SE, et al. Ossification of the posterior longitudinal ligament. Results of anterior cervical decompression and arthrodesis in sixty-one North American patients. Journal of Bone and Joint Surgery America. 2005;87(3):610-615. doi:10.2106/JBJS.C.01711
[6] Chen Y, Guo Y, Chen D, et al. Diagnosis and surgery of ossification of posterior longitudinal ligament associated with dural ossification in the cervical spine. European Spine Journal. 2009;18:1541-1547. doi:10.1007/s00586-009-1029-2
[7] Ferrante E, Ferrarini M, Castelli P, et al. Open trial of acetazolamide-topiramate for the treatment of idiopathic intracranial hypertension. Neurological Sciences. 2006;27(5):327-329. doi:10.1007/s10072-006-0727-3
[8] Bunge RP, Puckett WO, Becerra JL, et al. Observations on the pathology of human spinal cord injury. A review and classification of 22 new cases with details from a case of chronic cord compression with extensive focal demyelination. Advances in Neurology. 1993;59:75-89.
| How to Cite this article: Vatkar A, Kale S, Sonawane A. Recurrent Pseudomeningocele Following Surgery for Cervical Intramedullary Subependymoma: A Complex Case Report. Journal of Orthopaedic Complications. September-December 2025;2(3):28-32. |