Pedicle Screw Cut-Out Following Two-Level MIS TLIF: A Case Report and Lessons in Revision Strategy
Vol 2 | Issue 2 | May-August 2025 | page: 11-13 | Arvind Vatkar, Sachin Kale, Sushant Srivastava, Abhishek Bhati, Aditya Vyas, Ashok Shyam
Submitted Date: 02-02-2025, Review Date: 26-02-2025, Accepted Date: 22-04-2025 & Published Date: 10-07-2025
https://doi.org/10.13107/joc.2025.v02.i02.24
Authors: Arvind Vatkar [1], Sachin Kale [2], Sushant Srivastava [1], Abhishek Bhati [1], Aditya Vyas [1], Ashok Shyam [3]
[1] Director, Jupiter Hospital, Eastern Expressway, Thane, Maharashtra, India.
[2] Department of Orthopaedics, D.Y Patil School of Medicine and Hospital, Navi Mumbai, Maharashtra, India.
[3] Department of Orthopaedics, Sancheti Institute for Orthopaedics and Rehabilitation, Pune, Maharashtra, India
Address of Correspondence
Dr. Arvind Vatkar,
Director, Jupiter Hospital, Eastern Expressway, Thane, Maharashtra, India.
E-mail: vatkararvind@gmail.com
Abstract
Background: Pedicle screw loosening and cut-out are known complications of spinal fusion, often necessitating revision surgery. This case highlights challenges in screw fixation in a patient with potential bone quality concerns.
Case Report: A 41-year-old male with prior cranial surgeries and chronic lumbar stenosis underwent two-level MIS TLIF (L4-L5, L5-S1). Intraoperatively, L4 screw fixation was unstable, requiring upsizing. At four weeks post-op, he developed severe back pain and radiculopathy due to L4 screw cut-out. Revision involved screw removal and rod shortening (L5-S1 only), with subsequent pain relief.
Conclusion: Careful screw trajectory so that rods are correctly aligned and consideration of bone quality are crucial in spinal fusion. Early recognition and revision of failed fixation can prevent nerve damage.
Keywords:
Introduction
Posterior stabilisation using pedicle screws and rods is a well-established gold standard method for spine fixation that is used during treatment for spinal instabilities, malformation, degeneration, infection, and tumours [1]. But complications such as screw loosening and cut-out can occur although rare, particularly in osteoporotic bone or with technical errors [2] which can jeopradise structural integrity of fixation and also neural structures [3]. This case report discusses a 41-year-old male who developed L4 screw cut-out after a two-level MIS TLIF, necessitating revision surgery. The report emphasises risk factors, that unilateral pedicle screw fixation can suffice for degenerative spinal disorders.
Case Report
A 41-year-old male with hypertension and a history of suboccipital craniotomy (with residual slurred speech and gait disturbance) presented with chronic low back pain, bilateral radiculopathy (left > right), and neurogenic claudication (100-meter walking distance). MRI revealed severe stenosis at L4-L5 and L5-S1.
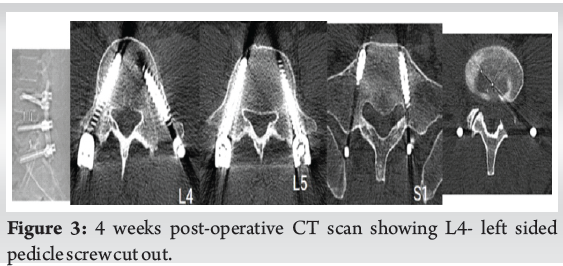
X-ray of lumbar-sacral spine with flexion and extension views suggested instability, with MRI scan showing significant stenosis at L45 and L5S1 levels as seen in Figure 1.
Initial Surgery (Two-Level MIS TLIF) entailed a posterior minimally invasive technique using intraoperative C-arm.
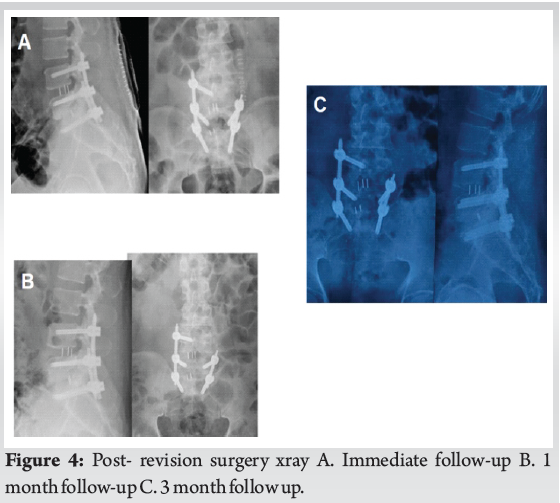
L4-L5 TLIF was done with cage insertion from the left side, as stenosis was more on the left side, as suggested by MRI. On the other hand, the L5S1 level TLIF cage was inserted from the right side as seen in the immediate post-operative x-ray Figure 2.
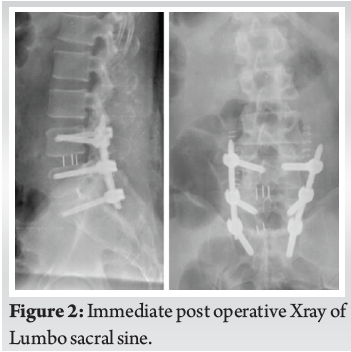
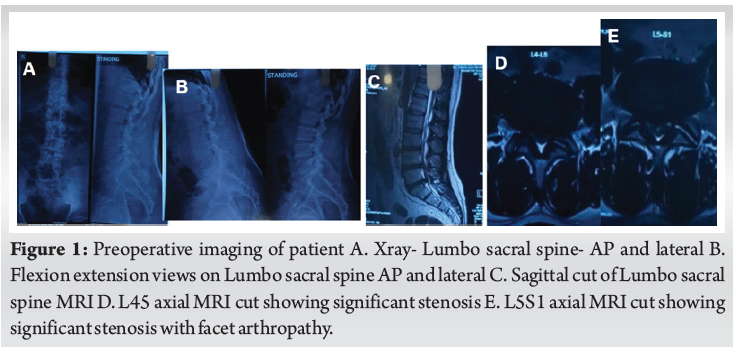
Intraoperative Challenges was while tightening the rods on left side, L4 left pedicle screw felt loose, hence was replaced with a 7.5 mm screw. L4 tulip misalignment required rod repositioning. The radicular pain patient had preoperatively decreased significantly; however, at four weeks, he developed severe left-sided back pain and left leg radiculopathy on weight bearing. CT scan imaging confirmed L4 screw cut-out on axial scans as seen in figure 3. Patient was conselled and posted for revision Surgery, in which removal of loose L4 screw was done and a short rod construct on Left side was done with levels only fixing L5 and S1 pedicle screws. The patient had significant pain relief post-surgery and was mobilised with a frame-type lumbo-sacral belt on the next day of surgery. The patient experienced complete resolution of radiculopathy, as confirmed by the final postoperative x-ray and follow-up x-rays at 1 month and 3 months, which showed good fusion and stability, as seen in Figure 4.
Discussion
The discussion discusses the lateral pedicle screw blowout, a critical complication in spine surgery, especially in minimally invasive spine surgery (MISS) due to its unique technical and biomechanical challenges. It explores its mechanisms, risk factors, clinical implications, mitigation strategies, and future directions, backed by peer-reviewed literature.
In MISS, pedicle screws are placed percutaneously and rods are reduced to correct alignment or deformity. Several mechanisms contribute to lateral pedicle blowout, including excessive reduction forces, suboptimal screw placement, thinner pedicle anatomy and bone quality, and deformity correction. Forces exceeding 200 N during rod reduction increase the risk of pedicle wall failure, especially during deformity correction [4]. Research shows higher breach rates in minimally invasive surgery (MISS) compared to open surgery due to reliance on imaging. Smaller, rotated pedicles on the concavity face a higher blowout risk during rod reduction in scoliosis cases [5].
MISS (Minimally Invasive Surgical Technique) is a surgical technique that involves small incisions and limited access, which can lead to a higher complication rate. Key risk factors include limited visualisation, technical challenges, and patient factors like age over 65 or complex deformities. Lateral blowout can compromise construct stability, cause injury to adjacent structures, require revision, and rarely remain asymptomatic [6]. Mitigation strategies include preoperative planning, intraoperative navigation, optimised surgical techniques, bone quality enhancement, and surgeon training.
In a prospective randomised trial by cheng et al, 48 patients underwent transforaminal lumbar interbody fusion (TLIF) for lumbar foraminal stenosis. They were compared to unilateral (UPSF) or bilateral pedicle screw fixation (BPSF). Outcomes were examined by VAS, ODI, and radiographic parameters (foraminal height, disc space height, segmental lordosis, fusion rates), and both groups exhibited considerable improvements, with no significant intergroup differences. UPSF resulted in shortened operation times and reduced blood loss. The study suggests that UPSF, with sufficient cage support, offers similar stability and fusion as BPSF, making it a less intrusive choice for TLIF [7].
On the same lines, rather than extending the fixation one level up, we considered having just fixation of L45 only on the right side. This is the first case report in literature mentioning lateral screw cut out in lumbar spine, which has been managed by unilateral pedicle screw fixation TLIF.
Conclusion
This case underscores the importance of meticulous screw placement and preoperative bone assessment. When screw cut-out occurs, prompt revision with a tailored construct can restore function and alleviate symptoms.
Clinical Message
– Surgeons should assess bone quality preoperatively, especially in patients with prior neurosurgical interventions.
– If screw purchase is suboptimal intraoperatively, alternative fixation methods (e.g., cement augmentation, higher level screw insertion, ) should be considered.
– Early revision with a modified construct can resolve instability and symptoms.
References
1. Chong XL, Kumar A, Yang EWR, Kaliya-Perumal AK, Oh JYL. Incidence of pedicle breach following open and minimally invasive spinal instrumentation: A postoperative CT analysis of 513 pedicle screws applied under fluoroscopic guidance. Biomedicine (Taipei) [Internet]. 2020 Jun 5;10(2):30–5. Available from: http://dx.doi.org/10.37796/2211-8039.1016
2. Cook SD, Salkeld SL, Stanley T, Faciane A, Miller SD. Biomechanical study of pedicle screw fixation in severely osteoporotic bone. Spine J [Internet]. 2004 Jul-Aug;4(4):402–8. Available from: http://dx.doi.org/10.1016/j.spinee.2003.11.010
3. Kaliya-Perumal AK, Charng JR, Niu CC, Tsai TT, Lai PL, Chen LH, et al. Intraoperative electromyographic monitoring to optimize safe lumbar pedicle screw placement – a retrospective analysis. BMC Musculoskelet Disord [Internet]. 2017 May 30;18(1):229. Available from: http://dx.doi.org/10.1186/s12891-017-1594-1
4. Lai DM, Shih YT, Chen YH, Chien A, Wang JL. Effect of pedicle screw diameter on screw fixation efficacy in human osteoporotic thoracic vertebrae. J Biomech [Internet]. 2018 Mar 21;70:196–203. Available from: http://dx.doi.org/10.1016/j.jbiomech.2017.10.009
5. Anekstein Y, Mirovsky Y, Arnabitsky V, Gelfer Y, Zaltz I, Smorgick Y. Reversing the concept: correction of adolescent idiopathic scoliosis using the convex rod de-rotation maneuver. Eur Spine J [Internet]. 2012 Oct;21(10):1942–9. Available from: http://dx.doi.org/10.1007/s00586-012-2355-3
6. Perna F, Borghi R, Pilla F, Stefanini N, Mazzotti A, Chehrassan M. Pedicle screw insertion techniques: an update and review of the literature. Musculoskelet Surg [Internet]. 2016 Dec;100(3):165–9. Available from: http://dx.doi.org/10.1007/s12306-016-0438-8
7. Cheng X, Zhang K, Sun X, Tian H, Zhao C, Zhao J. Unilateral versus bilateral pedicle screw fixation with transforaminal lumbar interbody fusion for treatment of lumbar foraminal stenosis. Spine J [Internet]. 2022 Oct;22(10):1687–93. Available from: http://dx.doi.org/10.1016/j.spinee.2022.05.011
| How to Cite this article: Vatkar A, Kale S, Srivastava S, bhati A, Vyas A, Shyam A | Pedicle Screw Cut- Out Following Two-Level MIS TLIF: A Case Report and Lessons in Revision Strategy | Journal of Orthopaedic Complications | May-August 2025;2(2):11-13.
|