Fixing the Edge: A Cautionary Tale of Implant Selection in Lateral Clavicle Fractures – A Case Report
Vol 2 | Issue 2 | May-August 2025 | page: 4-7 | J S R G Saran, Varun D, Wasal Sartaj, Yuvan B, Praneeth D V S, Hithyshi Datt
Submitted Date: 24-03-2025, Review Date: 10-04-2025, Accepted Date: 13-05-2025 & Published Date: 01-06-2025
https://doi.org/10.13107/joc.2025.v02.i02.20
Authors: J S R G Saran [1], Varun D [1], Wasal Sartaj [1], Yuvan B [1], Praneeth D V S [1], Hithyshi Datt [1]
[1] Department of Orthopaedics, M S Ramaiah University of Applied Sciences, Bengaluru, Karnataka, India.
Address of Correspondence
Dr. J S R G Saran,
Department of Orthopaedics, M S Ramaiah University of Applied Sciences, Bengaluru, Karnataka, India.
Email: jsaran868@gmail.com
Abstract
Lateral end clavicle fractures represent a complex subset of shoulder injuries due to their anatomical location and inherent instability. Unstable or displaced fractures frequently require surgical intervention to prevent non-union and restore shoulder function. This case report describes a 47-year-old male with a history of type 2 diabetes mellitus and hypertension who presented with an unstable lateral end clavicle fracture following a road traffic accident. Initial surgical fixation was performed using a midshaft pre-contoured locking plate. Despite initial stability, implant failure occurred by post-operative day five, presenting as pain and plate lift-off on radiographs. Revision surgery involved the use of a locking clavicle hook plate, which provided improved fixation and acromio-clavicular joint support. The patient had an uneventful recovery but was lost to follow-up. This case highlights the importance of appropriate implant selection based on fracture morphology, particularly in cases with small or comminuted distal fragments. Locking plates may not always provide sufficient stability in such scenarios. Hook plates, despite their known complications, can be a valuable alternative. Individualized treatment planning and biomechanical understanding are essential for optimal outcomes in complex lateral end clavicle fractures.
Keywords: Lateral end clavicle fractures, Implant failure, Hook plate
Introduction
Clavicle fractures are common orthopaedic injuries, with lateral end fractures accounting for approximately a quarter of the cases. These fractures often present significant treatment challenges due to their anatomical complexity and potential instability. While stable, non-displaced fractures may be managed conservatively, unstable patterns frequently require surgical intervention to prevent non-union. Various fixation methods have been employed, including locking plates and hook plates, each with specific indications and limitations. This case report describes a 47-year-old male with an unstable lateral end clavicle fracture, initially managed with a locking plate that failed post-operatively, necessitating revision with a hook plate. The case highlights the importance of individualized implant selection and pre-operative planning in managing complex lateral end clavicle fractures.
Case Presentation:
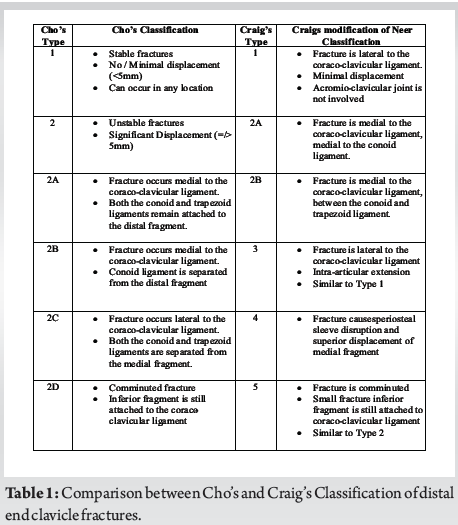
A 47-year-old male with a medical history of type 2 diabetes mellitus and hypertension presented to the emergency department following a road traffic accident, complaining of acute, sharp-shooting pain over the anterosuperior aspect of his left shoulder, accompanied by an inability to move the joint. On clinical examination, there was localized tenderness medial to the left acromio-clavicular (AC) joint, with swelling and the movement at the shoulder joint was restricted due to pain. No visible deformity was noted. A plain radiograph revealed a fracture of the lateral end of the clavicle, which came under Type 5 in Craig’s modification of Neer classification and Type 2D in Cho’s system. Given the patients’ high activity level, surgical intervention was deemed appropriate.
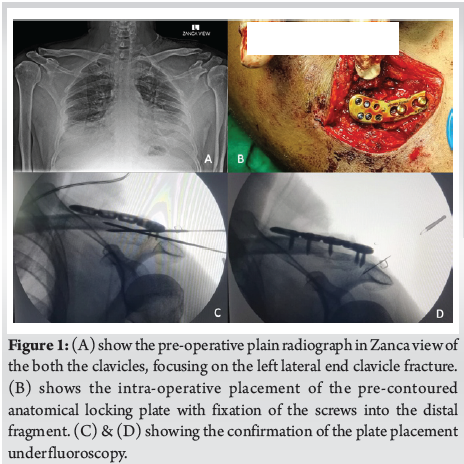
Under general anaesthesia, the patient was positioned supine and 20 degrees head-end elevation, with a bolster placed below the left shoulder making the clavicle prominent. An 8 centimetre incision was made over the left clavicle. After careful dissection, the fracture site was visualized, revealing a comminuted lateral end clavicle fragment with an intact AC joint, which was marked intra-operatively using an 18-gauge needle. Fracture reduction was achieved using reduction clamps and Kirschner wires. A midshaft pre-contoured 4-hole locking clavicle plate was applied to secure the fracture and fixation was confirmed under fluoroscopy. The surgical site was closed in layers (Fig. 1).
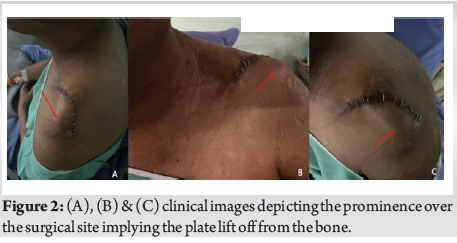
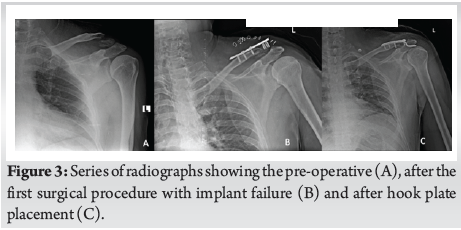
In the immediate post-operative period, the patient remained stable and was advised strict shoulder immobilization. However, by post-operative day five, he reported renewed pain over the same region and noticed a palpable bump over the clavicle (Fig. 2). Repeat radiographs revealed implant failure due to plate lift-off. The patient was then scheduled for a revision surgery. During the second procedure, the failed plate was removed and replaced with a 4-hole locking clavicle hook plate to provide better fixation and two-plane stability. The post-operative course was uneventful and the patient was gradually started on a guarded physiotherapy regimen (Fig. 3). No further complications or implant issues were reported, although the patient was subsequently lost to follow-up.
Discussion:
Clavicle fractures are among the most frequently encountered orthopaedic injuries, with an estimated incidence of 30 per 100,000 individuals, accounting for approximately 2.6% to 4.0% of all fractures [1]. The midshaft region is most commonly affected, comprising 70% to 80% of cases, while fractures of the lateral and medial thirds represent approximately 28% and 3%, respectively [2, 3]. Lateral end clavicle fractures, in particular pose unique treatment challenges due to their anatomical complexity and higher risk of instability. Various classification systems have been proposed to better guide management. Neer’s classification, later modified by Craig and more recently Cho’s classification (2018), are among the most widely used (Table 1) [4, 5]. In the present case, the fracture was categorized as Type 5 in Craig’s modification of Neer and Type 2D in Cho’s system.
While conservative treatment is often sufficient for stable, non-displaced lateral clavicle fractures, unstable patterns typically require surgical intervention to avoid non-union. Dodia et al. reported a 50% non-union rate in unstable Neer-type fractures treated conservatively, whereas surgical fixation yielded superior union rates using plates and cortico-cancellous screws [6]. Given these considerations, operative management was chosen for our patient.
A variety of surgical options are available for lateral clavicle fractures, ranging from tension band wiring to plate fixation. Locking plates are frequently employed due to their biomechanical stability, minimal cortical bone disruption and suitability for minimally invasive techniques [7]. Anatomically contoured plates with lateral screw clusters allow for effective stabilization of small distal fragments and often incorporate features for CC ligament augmentation. In cases involving coraco-clavicular (CC) ligament disruption as seen in Neer Type 2B or Type 5, supplemental CC fixation is recommended as locking plates alone may not provide adequate vertical stability [8]. Superior placement of the plate has been shown to offer optimal mechanical strength. Nevertheless, limitations include difficulty in achieving secure fixation in cases of comminuted fractures and the risk of implant prominence, sometimes necessitating hardware removal [9]. In our case also the same principle was advocated.
Other plating systems including reconstruction plates, limited-contact dynamic compression plates and T-plates have also demonstrated favourable clinical outcomes, though direct comparative data with locking plates are limited. In osteoporotic bone, locking plates offer superior fixation and reduce the risk of screw loosening. However, in elderly patients, complications related to plating may be more common compared to intramedullary options such as Knowles pinning [10].
Hook plates provide reliable fixation in cases with small distal fragments or concomitant CC ligament injury by offering both horizontal and vertical stability [11]. They are associated with high union rates but also carry risks, which mainly inlcude acromial erosion, subacromial impingement, joint arthrosis and implant-related complications, often necessitating removal after union [12]. As such, their use is best reserved for select indications where alternative fixation methods are not feasible.
In our case, fixation was initially attempted using a pre-contoured anatomical locking plate. However, due to insufficient purchase on the small distal fragment, the construct failed, resulting in plate lift-off and implant prominence. Given the instability and fracture morphology, conversion to a hook plate was performed, providing the necessary fixation and acromio-clavicular joint support. This case underscores the importance of meticulous pre-operative planning and appropriate implant selection tailored to the specific fracture characteristics and patient needs.
There are also emerging techniques that have further expanded treatment options. Ahmed et al. described a modified surgical approach incorporating suture anchors, suture buttons and supplemental acromio-clavicular joint fixation for unstable lateral end clavicle fractures, demonstrating improved union and functional outcomes with minimal complications [13]. Additionally, minimally invasive techniques are gaining prominence. Solanki et al. reported successful arthroscopic management of a displaced lateral end clavicle fracture using FiberWire and FiberTape, resulting in 100% union and excellent clinical outcomes with minimal morbidity [14]. These procedures can also be employed during the pre-operative planning as well, but the technical expertise, affordability and availability of the implants should be taken into consideration.
Conclusion:
Lateral end clavicle fractures, particularly unstable patterns, require careful assessment and tailored surgical management to ensure optimal outcomes. Although locking plates are a widely accepted fixation method offering strong biomechanical support, their effectiveness may be limited in cases with small or comminuted distal fragments. This case demonstrates that inadequate implant purchase can lead to early failure, emphasizing the need for appropriate implant selection based on fracture morphology. The successful revision with a hook plate provided the necessary stability and highlights its role as a valuable alternative in select scenarios. Ultimately, meticulous pre-operative planning, an understanding of implant biomechanics and individualized treatment strategies are essential in achieving stable fixation and favourable clinical outcomes in complex clavicle fractures.
References
1. Frima H, van Heijl M, Michelitsch C, van der Meijden O, Beeres FJP, Houwert RM, et al. Clavicle fractures in adults; current concepts. Eur J Trauma Emerg Surg [Internet]. 2020;46(3):519–29. Available from: http://dx.doi.org/10.1007/s00068-019-01122-4
2. Dong D, Yu M, Gu G. Simultaneous bilateral midshaft clavicle fractures with unilateral dislocation of the acromio-clavicular joint: A case report: A case report. Medicine (Baltimore) [Internet]. 2017;96(21):e6975. Available from: http://dx.doi.org/10.1097/MD.0000000000006975
3. Robinson CM. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br [Internet]. 1998;80(3):476–84. Available from: http://dx.doi.org/10.1302/0301-620x.80b3.8079
4. Craig EV. Fractures of the clavicle. In: Rockwood CA, Matsen FA, editors. The shoulder. Philadelphia: WB Saunders; 1990. pp. 1109–1193.
5. Kim D-W, Kim D-H, Kim B-S, Cho C-H. Current concepts for classification and treatment of lateral end clavicle fractures. Clin Orthop Surg [Internet]. 2020;12(2):135–44. Available from: http://dx.doi.org/10.4055/cios20010
6. Dodia AV, Dodia PA, Dodia A, Shah P. Outcomes of fractures of lateral end of clavicle using different modalities of management. 2017; Available from: https://www.ijos.co.in/journal-article-file/3827
7. Perren SM. Evolution and rationale of locked internal fixator technology. Introductory remarks. Injury. 2001;32 Suppl 2:B3-9.
8. Furuhata R, Matsumura N, Udagawa K, Oki S, Morioka H. Residual coracoclavicular separation after plate fixation for lateral end clavicle fractures: comparison between fracture patterns. JSES Int [Internet]. 2021;5(5):840–5. Available from: http://dx.doi.org/10.1016/j.jseint.2021.04.017
9. Davis BP, Shybut TB, Coleman MM, Shah AA. Risk factors for hardware removal following operative treatment of middle- and distal-third clavicular fractures. J Shoulder Elbow Surg [Internet]. 2021;30(3):e103–13. Available from: http://dx.doi.org/10.1016/j.jse.2020.06.034
10. Muthu S, Annamalai S, Kandasamy V. Lateral clavicle fracture-plating options and considerations. World J Clin Cases [Internet]. 2024;12(6):1039–44. Available from: http://dx.doi.org/10.12998/wjcc.v12.i6.1039
11. Asadollahi S, Bucknill A. Hook plate fixation for acute unstable lateral end clavicle fracture: A systematic review and Meta-analysis. J Orthop Trauma [Internet]. 2019;33(8):417–22. Available from: http://dx.doi.org/10.1097/BOT.0000000000001481
12. Shimpuku E, Uchiyama Y, Imai T, Takatori N, Watanabe M. Relationship between subacromial bone erosion and hook position of clavicular plate in lateral end clavicle fractures. J Orthop Trauma [Internet]. 2022;36(6):e243–9. Available from: http://dx.doi.org/10.1097/BOT.0000000000002301
13. Ahmed AF, Salameh M, Kayali H, Hantouly A, Darwiche A. Open reduction and tunneled suspensory fixation for lateral end of clavicle fractures: surgical technique. JSES Rev Rep Tech [Internet]. 2022;2(3):345–9. Available from: http://dx.doi.org/10.1016/j.xrrt.2022.02.010
14. Solanki KP, Soundarapandian RS, Manoharan S. A novel surgical technique for arthroscopic fixation of lateral end clavicle fracture using FiberWire and FiberTape. Journal of Arthroscopic Surgery and Sports Medicine [Internet]. 2020;1(199):199–206. Available from: http://dx.doi.org/10.25259/jassm_27_2020
| How to Cite this article: Saran JSRG, Varun D, Sartaj W, B Yuvan, D V S Praneeth, Datt H | Fixing the Edge: A Cautionary Tale of Implant Selection in Lateral Clavicle Fractures – A Case Report | Journal of Orthopaedic Complications | May-August 2025;2(2):04-07. |