Avoiding FNS in Osteoporotic Neck of Femur Fractures: Lessons from Clinical Practice
Vol 2 | Issue 2 | May-August 2025 | page: 14-18 | Sachin Kale, Arvind Vatkar, Sushant Srivastava, Ojasv Gehlot, Gursimran Singh, Nikhil Makhija
Submitted Date: 20-3-2025, Review Date: 12-04-2025, Accepted Date: 22-05-2025 & Published Date: 10-07-2025
https://doi.org/10.13107/joc.2025.v02.i02.26
Authors: Sachin Kale [1], Arvind Vatkar [2], Sushant Srivastava [1], Ojasv Gehlot [1], Gursimran Singh [1], Nikhil Makhija [1]
[1] Department of Orthopaedics, D.Y Patil School of Medicine and Hospital, Navi Mumbai, Maharashtra, India.
[2] Department of Orthopaedics, MGM Medical College, Navi Mumbai, Maharashtra, India.
Address of Correspondence
Dr. Sachin Kale,
Department of Orthopaedics, D.Y Patil School of Medicine and Hospital, Navi Mumbai, Maharashtra, India.
E-mail: sachinkale@gmail.com
Abstract
Background: The Femoral Neck System (FNS) is a newer, minimally invasive fixation device that offers angular and rotational stability in femoral neck fractures. While it has shown promising outcomes in younger patients with good bone stock, its application in elderly patients with osteoporosis remains controversial due to compromised implant anchorage and increased risk of mechanical failure.
Case Report: We present the case of a 70-year-old male with a displaced Pauwels Type III femoral neck fracture following a trivial fall. The patient, with known osteoporosis, was managed with internal fixation using the FNS. Despite initial satisfactory radiographs, the patient developed progressive pain and functional limitations over 5 months. Follow-up imaging revealed non-union, varus collapse, and implant cut-out, necessitating revision to total hip replacement (THR). Intraoperatively, severe osteopenia, femoral head changes, and failed implant integration were observed, complicating the salvage procedure.
Discussion: This case underscores the limitations of FNS in osteoporotic bone. Biomechanical stability offered by FNS is contingent on good trabecular support, which is often lacking in geriatric hips. Implant failure in such cases may result in prolonged morbidity, increased revision burden, and poor outcomes. Salvage procedures like THR can be technically demanding due to bone loss, deformity, and prior implant tracks. The decision-making process must consider patient age, bone quality, and functional expectations.
Conclusion: FNS may not be the ideal fixation method for elderly osteoporotic patients with femoral neck fractures. In this population, arthroplasty provides more predictable and durable outcomes, especially when bone quality is poor. Appropriate preoperative planning, bone quality assessment, and individualized implant selection are essential to avoid fixation failure and reduce revision rates.
Keywords: Femoral Neck System (FNS), Osteoporosis, Femoral neck fracture, Implant failure, Avascular necrosis, Total hip replacement, Elderly, Pauwels Type III fracture, Biomechanics, Orthopaedic implant selection
Introduction
Introduction to FNS and its Controversy Fractures of the femoral neck are common in the elderly and are often compounded by osteoporosis. The FNS is a newer, minimally invasive fixation device that has gained popularity due to its biomechanical advantages and promising early results in young adults with good bone stock. However, its application in elderly patients with osteoporotic bone remains controversial. Poor bone quality compromises the anchorage and stability of the implant, which can lead to severe complications such as implant cut-out, varus collapse, and fixation failure. The report critically examines these limitations and underscores the importance of selecting patients appropriately and planning individualized treatment.
Case Report:
This case report addresses the evolving management of femoral neck fractures in the elderly, particularly those with osteoporosis. It raises questions about the Femoral Neck System (FNS), asking if there is “Misplaced Confidence” in its application for this patient group.
History- A 70-year-old male presented to the emergency department after a fall at home, approximately two hours prior. He reported severe pain in the right hip and an inability to bear weight. The fall directly impacted his hip. He denied head injury, loss of consciousness, or other systemic symptoms. The patient had a known history of osteoporosis and was being intermittently treated with calcium and vitamin D supplements. He had no prior hip surgeries or known malignancies.
Clinical Examination Findings upon examination of the right lower limb, the following was noted:
Attitude of the Limb: The right lower limb was in external rotation and slight flexion at the hip, with noticeable shortening compared to the contralateral side.
Swelling and Deformity: Mild diffuse swelling over the hip region was present, along with a visible deformity and palpable bony irregularity in the femoral neck area.
Tenderness: Severe tenderness was elicited over the anterior hip joint line and greater trochanter.
Movements: Active movements were not possible due to pain, and passive movements were painful and grossly restricted at the hip joint.
Shortening: Apparent and true shortening of approximately 2.5–3 cm was observed, alongside an external rotation deformity.
Neurovascular Status: Intact distally, with palpable and equal dorsalis pedis and posterior tibial pulses bilaterally. No sensory or motor deficit was noted.
Functional Impact: The patient was unable to stand or bear weight on the right limb and required two-person assistance to change position in bed.
Investigations:
Initial radiological findings X-rays of the pelvis with both hips (AP and lateral views) revealed (Fig. 1).
A displaced intracapsular fracture of the right femoral neck.
The fracture line was transverse with a vertical orientation, categorised as a Pauwels Type III.
There was a loss of continuity with medial breaking, absence of calcar support, and no impaction.
The proximal femur showed trabecular thinning and generalised osteopenia, strongly suggesting osteoporotic bone.
No signs of pathological lesion or prior implants were observed.
Postoperative Course and Complications (Fig. 2). Initial postoperative radiographs demonstrated adequate reduction and proper placement of the FNS implant within the femoral head and neck.
However, at five months post-surgery, despite the implant initially holding well, the patient experienced mild pain. Follow-up (Fig. 3) radiographs revealed concerning findings.
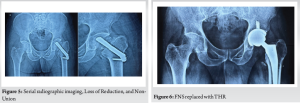
Loss of Reduction and Non-Union: The fracture line remained visible across serial films, with no evidence of trabecular bridging or cortical continuity, indicating an established non-union. Mild rounding of the proximal femoral fragment further supported this diagnosis. (Fig. 4)

Implant Cut-out: Progressive superior migration of the fixation screw was observed, breaching the subchondral bone of the femoral head. This indicated mechanical failure and loss of purchase, consistent with implant cut-out. (Fig. 5)
Femoral Head Changes: Early sclerotic changes were noted in the femoral head, raising suspicion for evolving avascular necrosis (AVN), likely exacerbated by delayed fixation and mechanical failure.
Challenges in Treatment Following FNS Failure– The case highlighted several significant challenges encountered in treating this patient after FNS failure:
Implant Failure in Osteoporotic Bone: The FNS, while minimally invasive and biomechanically superior in younger patients, proved less effective in osteoporotic bone. The osteoporotic femoral neck failed to provide adequate hold for the bolt and screws, leading to loss of reduction, varus collapse, implant migration or cut-through, nonunion, or avascular necrosis.
Persistent Pain and Loss of Function: The patient experienced worsening hip pain, inability to bear weight, and loss of mobility, significantly diminishing quality of life and increasing dependency.
Difficulties in Salvage Surgery: Removing the FNS implant was technically demanding due to the potential for iatrogenic damage and risk of additional bone loss. Residual fracture site deformity, sclerotic margins, and avascular bone complicated reconstruction.
Poor Bone Stock: Chronic disuse, previous surgical trauma, and osteoporosis contributed to a loss of structural integrity, with thin cortices making secure fixation during salvage procedures (e.g., arthroplasty) more difficult.
Decision-Making in Revision: The choice between osteosynthesis revision and conversion to arthroplasty depended on the patient’s age, bone quality, fracture type, and mobility demands. In most elderly osteoporotic patients, arthroplasty is favoured over repeat fixation due to poor healing potential.
Challenges in Arthroplasty Post-FNS Failure: Proximal femur deformity, implant tracks, and sclerosed bone could affect prosthesis alignment. Cemented hemiarthroplasty or total hip replacement (THR) was often required, demanding special care to avoid intraoperative fractures, stem subsidence, and dislocation (especially with compromised abductor function).
Increased Surgical Risk: Elderly patients with comorbidities (e.g., diabetes, hypertension, cardiac disease) are at higher risk for perioperative complications (DVT, pneumonia, delirium), delayed wound healing, or infection.
Surgical Procedure: FNS Replaced with THR The patient underwent a total hip replacement (THR) to address the FNS failure and non-union.
Anesthesia and Positioning: Spinal anesthesia was administered, and the patient was positioned in a lateral decubitus position.
Surgical Approach: A posterior (Moore/Southern) approach was taken, involving an incision centered over the greater trochanter, extending proximally and distally.
Implant Removal: The FNS components were carefully identified and extracted using the manufacturer’s tools, with care taken to minimise further bone loss. Curettage and lavage cleared fibrous tissue from the nonunion site.
Femoral Head Resection: The femoral head was resected, and the femoral canal was prepared using rasps or broaches.
Trial Reduction: A trial head and femoral stem were used to assess leg length, stability, and soft tissue tension.
Final Implant Insertion: An uncemented femoral stem was definitively inserted, and a head of appropriate size was assembled and reduced into the acetabulum.
Closure: The joint capsule was repaired, and short external rotators were reattached. Layers were closed, and a drain was placed. The patient was mobilised with a walker on day 1 post-surgery.
Post-operative Course (after THR)- Post-operative X-rays (Fig. 6) were acquired to validate implant positioning. Range of motion exercises began on day 1, with weight-bearing initiated on day 3. Pain management, DVT prophylaxis, and physiotherapy were all initiated.
Key Points from the Case Report
Patient Factors Matter: Elderly and osteoporotic patients have compromised bone quality, making internal fixation less reliable.
FNS Mechanism: While designed for minimally invasive fixation and offering angular stability, the FNS relies on good bone stock for optimal performance.
Biomechanical Limitations in Osteoporosis: Poor trabecular support in osteoporotic bone reduces implant hold, significantly increasing the risks of cut-out or implant migration.
High Risk of Failure: Clinical experiences and studies report increased rates of implant failure and nonunion in osteoporotic patients treated with FNS.
Alternative Strategies: Arthroplasty (hemi or total) offers better pain control, earlier mobilisation, and improved functional outcomes in geriatric patients.
Implant Choice Should Be Personalised: The selection of the implant must be guided by the patient’s age, bone quality, fracture pattern, and their mobility expectations.
Conclusion:
The Femoral Neck System represents a modern advancement in internal fixation for femoral neck fractures, but it is not ideal for elderly and osteoporotic patients. The success of this implant is heavily dependent on bone quality and mechanical stability, both of which are significantly compromised in geriatric hips. In such scenarios, arthroplasty remains the gold standard, providing superior long-term results, reducing reoperation rates, and facilitating early rehabilitation. The report emphasises that clinical judgment, proper evaluation, and individualised planning are essential to ensure optimal outcomes.
Learning Points
1. Avoid FNS in Poor Bone Stock: In osteoporotic bone, FNS may not provide adequate purchase, leading to failure.
2. Preoperative Assessment is Crucial: Assessing bone quality (e.g., via DEXA scan or intraoperative feel) should guide the decision between fixation and replacement.
3. Arthroplasty is Superior in the Elderly: Hemiarthroplasty or Total Hip Replacement offers a reliable and durable solution for older adults.
4. Minimise Reoperations: Choosing the correct primary procedure can avoid complications such as implant failure, nonunion, and the need for revision surgeries.
5. Biomechanics Matter: The angular stability offered by FNS cannot compensate for the absence of structural bone integrity in osteoporotic necks.
6. Multidisciplinary Care Benefits Recovery: Optimising nutrition, managing medical comorbidities, and providing physiotherapy all contribute to improved post-operative recovery in elderly patients.
References
1. Parker MJ, Gurusamy K. Internal fixation implants for intracapsular proximal femoral fractures in adults. Cochrane Database Syst Rev. 2006;(4):CD001467.
2. Palm H, Gosvig K, Krasheninnikoff M, Holck K, Jacobsen S, Gebuhr P. A new algorithm for hip fracture surgery. J Bone Joint Surg Br. 2006 Jul;88(7):916-21.
3. Zlowodzki M, Ayieni O, Petrisor BA, Bhandari M. Femoral neck shortening after internal fixation of femoral neck fractures. Orthop Clin North Am. 2009 Jan;40(1):373-84.
4. Stoffel K, Zderic I, Klos K, Gueorguiev B, Fuchs T. Biomechanical evaluation of the femoral neck system in unstable Pauwels III fractures: a comparison with the dynamic hip screw and cannulated screws. J Orthop Trauma. 2017 Mar;31(3):131-137.
5. Bhandari M, Devereaux PJ, Swiontkowski MF, Tornetta P, Obremskey W, Koval KJ, et al. Internal fixation compared with arthroplasty for displaced fractures of the femoral neck: a meta-analysis. J Bone Joint Surg Am. 2003 Sep;85(9):1673-81.
6. Damany DS, Parker MJ, Chojnowski A. Complications of intracapsular hip fractures in young adults. Acta Orthop Belg. 2005 Aug;71(4):389-94.
7. Zielinski SM, Keijsers NL, Praet SF, Heetveld MJ. Femoral neck shortening after internal fixation of a femoral neck fracture. Orthopaedics. 2013 Sep;36(9):e1115-20.
8. Slobogean GP, Sprague SA, Scott T, Bhandari M. Management of young femoral neck fractures: is there a consensus? Injury. 2015 Mar;46(3):435-40.
9. Knobe M, Drescher W, Heussen N, Sellei R, Pape HC. Is helical blade better than screw blade? Acta Orthop. 2012 Oct;83(5):481-6.
10. Vidyadhara S, Rao SK. One and two femoral neck screw fixation of femoral neck fractures in the elderly. Indian J Orthop. 2011 Jul;45(4):336-43.
11. Mardani-Kivi M, Karimi-Mobarakeh M, Keyhani S, Hoseini M. Comparison between hip arthroplasty and internal fixation for femoral neck fractures in elderly patients. Med Arch. 2016 Aug;70(4):274-7
12. Lee YK, Park CH, Kim JW, Moon KH, Ha YC, Koo KH. Implant-related complications after fixation of femoral neck fracture with FNS. Clin Orthop Surg. 2021 Dec;13(4):435-442.
13. Nauth A, Creek AT, Zlowodzki M, Waddell JP. Strategies for the management of proximal femoral fractures in the elderly: a review. Bone Joint J. 2015 Jul;97-B(7):866-73.
14. Zhang B, Wang Y, Xu B, Liu J. Efficacy of femoral neck system in elderly patients: a comparative study. J Int Med Res. 2020 Nov;48(11):1-10.
| How to Cite this article: Kale S, Vatkar A, Srivastava S, Gehlot O, Singh G, Makhija N | Avoiding FNS in Osteoporotic Neck of Femur Fractures: Lessons from Clinical Practice | Journal of Orthopaedic Complications | May-August 2025;2(2):14-18. |